The Emotions Of Motherhood — From The Start, Postpartum Doula
I want to highlight just a few of the data points here. The other data point I want to point out is that 10 women, 11% of respondents, experienced PMAD after their next (second or later) delivery. Of these 10 women, 3 of them had never experienced loneliness, baby blues, PPD, or other PMAD. This is something that is not often discussed – that it is actually possible to experience some sadness (somewhere on the scale between sadness to severe PMAD) after the second, third, fourth, etc. of giving birth without experiencing it during first birth
The second point I want to highlight is the 21 women who indicated that they experienced “undiagnosed postpartum depression after my first child.” So 21 of the 89 women, or 24% of the participants in this poll indicated that they probably experienced some type of postpartum depression for which they did not receive any type of care. This is substandard care. Lindsey shared her story with the group: “After my first, I definitely suffered from undiagnosed postpartum depression. Between her complete disinterest in breastfeeding and colic, I felt like she hated me. I felt like I failed because I couldn’t latch him and ended up pumping. With his colic making it almost impossible to sleep and him not being able to rest/figure out what was wrong didn’t help my ‘I’m a horrible mom’ complex. Because I active duty (Army) at the time, the thought of seeking help was terrifying because I knew the stigma associated with receiving treatment (especially for women) – which only added to the stress.”
There are many different factors that contribute to these feelings. Some of the factors are situational, while other factors are hormonal. From the information provided by the women in The Group, my own experience, and the experiences I have heard from others, I strongly believe that we need to better support the mental wellness of mothers of newborns/babies. Take Sara, for example. Sara probably did not meet the screening requirements because, as she said, “I really didn’t think I had anything because I never felt suicidal, just overwhelmed, alone, and frustrated with a child that wouldn’t stop crying . I think the lack of sleep played a big role in my ability to manage my emotions.” In this example, Sara doesn’t have severe PMAD, but she could definitely benefit from some attention to her mental health in those early days, weeks, and months with her babies.
I wonder how different the responses above would be if every mother cared for and monitored her mental health in the same capacity that we care for and monitor wet and dirty baby diapers.
Fortunately, changes are on the horizon. The American College of Obstetricians and Gynecologists (ACOG) recently issued a committee opinion on “Optimizing Postpartum Care” and is the first step necessary for profound changes in the standard of care for postpartum women. These include recommendations for more comprehensive prenatal screening for PMADs, earlier and potentially more frequent visits to care providers in the first days and weeks in the postpartum period, as well as more individualized care. This is a huge step forward and, although it is only a recommendation and not yet a policy, it is absolutely a step in the right direction to help catch these women who have suffered in silence.
There are dozens of books, websites, blogs, therapists, and other amazing resources available for self-help on the topic of maternal mental health. However, despite the abundance and availability of these resources, many of us mothers struggle to get the real support we need at a time when we need it most. Whether it’s because we’re so sad and anxious about leaving home or we feel like we’re alone and what we’re experiencing is something rare and we’re not sure where to start, America is struggling to really help. . I have high hopes for the improved future of maternal mental health care – it affects more than just the mother.
A Sequel to “Inside Out”
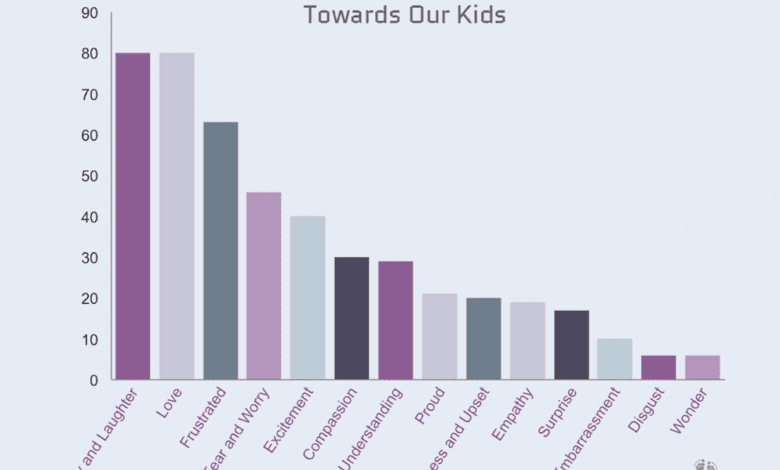
In fact, all the emotions of the mother do not only affect her. Research shows that a child’s emotional well-being is highly dependent on the mother and her emotional processes. In fact, M. Ann Easterbrooks and Zeynep Biringen wrote that “emotional availability is defined as the ‘connective tissue’ in mother-child relationships.” The topic of attachment and the feelings of the mother-child dyad. Good, bad, or indifferent, our children learn emotional intelligence, emotional regulation, and the basic expression of emotion from us!
So, that love that is felt deeper because of them, they learn how to feel the same love. And the fear and worry that surprised us, well, they learned that too. Yes, even the sadness. These feelings, each one of them, make us who we are. We all experience emotions – that’s the wonderful part of being human. How we handle them and react to them, now that is what makes us individual.
One last thought to leave you with. I do a lot of driving and, therefore, I listen to a lot of podcasts. One that I’m interested in recently came out of UC Berkely and is called The Science of Happiness. Specifically, about 2 weeks ago, I listened Episode 5: Walk Outside with Inside Out’s Pete Doctor. Walking outside AND learning more about the movie right from the director’s mouth?!?! Holy Vision, Batman! Yes Please!
Mr. Doctor’s revelation is too good, and too relevant, to summarize. Here is what he says:





