Placenta Previa: Symptoms, Diagnosis and Treatment

The placenta can be considered the powerhouse of pregnancy. It is an intricate network of vessels and tissues that nourishes and sustains the development of life.6 But what happens when the placenta is not located where it should be? Let’s discuss the symptoms and complications that can occur when the placenta blocks your baby’s exit from your uterus (placenta previa). We’ll also discuss whether there is a treatment for placenta previa and what questions to ask your doctor about it.
Placenta previa occurs when a developing position of the placenta completely or partially covers the cervical opening. Unfortunately, this blockage can prevent a safe path for vaginal delivery and increases the risk of dangerous bleeding during pregnancy. This condition affects approximately 0.3-2% of pregnancies in the third trimester.1
The good news? The placenta can migrate inside your uterus. Up to 90% of low-lying placenta previas resolve by delivery as the uterus enlarges and the placenta grows.1
There are three types of placenta previa:1
- Marginal or “low lying” placenta previa: It is a placenta that lies within 2 centimeters of the internal cervical opening. This type is the most likely to migrate away from the cervical opening, also called the cervical os.
- Partial placenta previa: The placenta partially blocks the internal cervical opening.
- Total or complete placenta previa: The placenta completely blocks the internal cervical opening.
A transvaginal ultrasound examination determines the position of your placenta in relation to the cervical os.1,4
Placenta previa can be diagnosed early in pregnancy by routine transvaginal ultrasound. A follow-up ultrasound between 28 and 32 weeks can determine if the placenta previa is persistent and likely to be stationary.1,4
Health care providers may suspect placenta previa if you develop painless, bright red vaginal bleeding during the second or third trimester. However, placenta previa is only one of several conditions that can cause vaginal bleeding in the next pregnancy. The cardinal placenta previa symptom of painless bleeding may begin after intercourse, after a vaginal examination, during childbirth, or for no apparent reason.1
Causes and Risk Factors
The causes of this condition are unknown. However, several risk factors have been identified:1
- Age more than 35 years old
- Multiple pregnancies
- Assisted reproductive technology
- smoking
- Cocaine use
- History of suction and curettage
- History of previous cesarean sections
- History of previous placenta previa
These risk factors can result in endometrial damage, uterine scarring, or abnormal placental blood flow.1 This affects how the placenta grows and connects within the uterus. Certain risk factors can increase the chance of developing this condition, but they do not guarantee its development.1
Placenta previa will change the care you receive during pregnancy and delivery, and significant complications are possible. Open communication with your obstetric provider is paramount. Here are the potential complications:
This condition can significantly increase the risk of preterm delivery. One study revealed that 3.5% of pregnancies were delivered before 28 weeks, 11.7% were delivered before 32 weeks, and 16.1% were delivered before 34 weeks.2
A baby born prematurely can have some complications depending on the gestational age. Sadly, placenta previa is associated with a three- to fourfold increase in infant mortality that is generally due to the risks associated with early preterm birth.1 Other risks for the newborn include:1
- Low birth weight
- Low APGAR score
- Respiratory distress syndrome
Fortunately, research has not found placenta previa to affect the baby’s growth.7
Bleeding from placenta previa can lead to life-threatening bleeding and occurs in about 60% of pregnancies complicated by placenta previa.2 Maternal hemorrhage can lead to:2
- Blood transfusion
- Admission to the intensive care unit
- Septicemia-bacterial infection of the blood
- Hysterectomy (removal of the uterus)
- Death
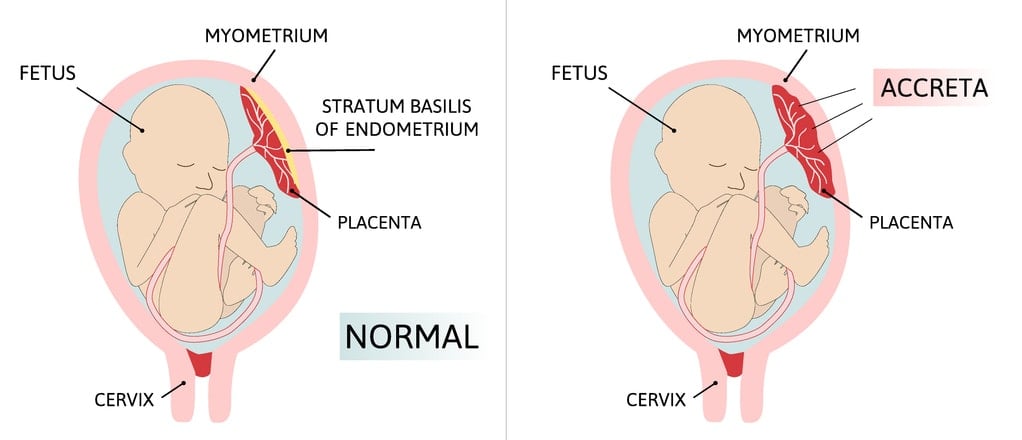
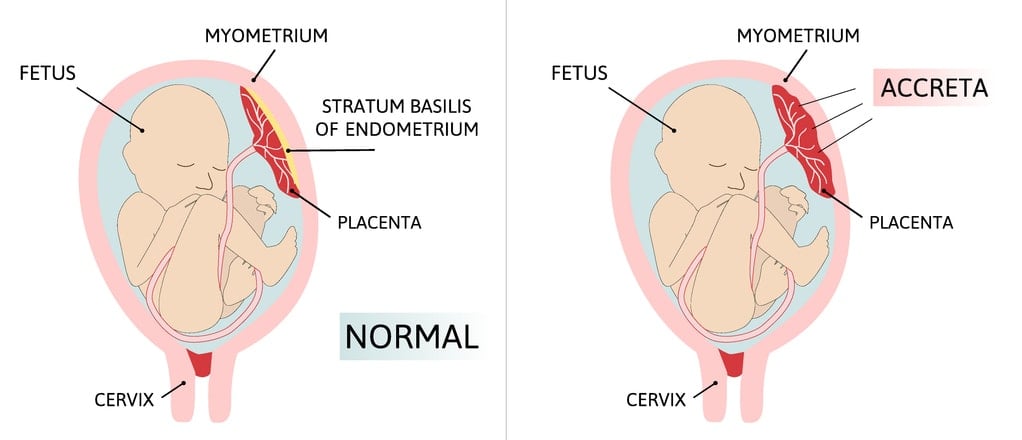
Placenta accreta spectrum (PAS) occurs when the placenta grows into the myometrium or inner lining of the uterus. You will have a greater risk of developing PAS if you have placenta previa.3
The placenta accreta spectrum describes the depth to which the placenta has grown into the myometrium. PAS greatly increases the pregnant parent’s risk for fatal hemorrhage, hysterectomy, and death.3 Additionally, if you have placenta previa and a history of a previous cesarean section, your risk of developing PAS increases with each cesarean section.3
Unfortunately, there is no confirmed treatment for placenta previa.3 It is a condition of active and prospective management. Medical intervention depends on the extent of placenta previa, the number of weeks pregnant, the presence of bleeding, the onset of labor, and any other complicating factors. The delivery plan for patients with this condition is cesarean section between 36-37 weeks of gestation.8
In the past, bed rest and pelvic rest (no intercourse) may have been considered placenta previa self-care. However, there is limited modern research to support the benefit of these restrictions.3 In fact, limiting physical activity can increase the risk of blood clots, bone loss, and a decrease in muscle mass.5 Your provider can adjust any “restrictions” based on your situation while taking into account the extent of the previa, week of pregnancy, and presence of bleeding.
Finding out you have placenta previa can be very difficult. You may have many questions to ask your obstetric provider. Here are some good things to start the conversation:2
- Is a vaginal birth possible with placenta previa?
- What symptoms of placenta previa during pregnancy require an immediate phone call and/or hospital visit?
- Will my delivery be scheduled, or will I wait for labor to begin?
- Will a blood transfusion be needed?
- Are options for anesthesia changing during delivery?
- What additional medical interventions can I expect? (example: two intravenous lines or prophylactic medication)
- How can I ensure proper bonding with my baby during and after cesarean delivery?
Complications of this condition can be serious, so life-saving measures and consent are likely to be an important part of your discussions with your obstetric provider.
Placenta previa, especially partial or complete placenta previa, has important implications for pregnancy and childbirth. Although there is no treatment for placenta previa, knowing the risks and potential outcomes of this condition can help you be better prepared. Don’t hesitate to talk to your obstetric provider about what to expect!





